Scientific Calendar December 2021
Which haemostasis tests would you consider as an early indicator of a disseminated intravascular coagulopathy (DIC) in patients with sepsis?
Which parameters are used to identify an overt DIC according to the ISTH DIC score?
Platelet count, prothrombin time, fibrin-degradation products / D-dimer, SOFA score and fibrinogen
Platelet count, prothrombin time, fibrin-degradation products / D-dimer and fibrinogen
Platelet count, prothrombin time and SOFA score
Congratulations!
That's the correct answer!
Sorry! That´s not completely correct!
Please try again
Sorry! That's not the correct answer!
Please try again
Notice
Please select at least one answer
Scientific background
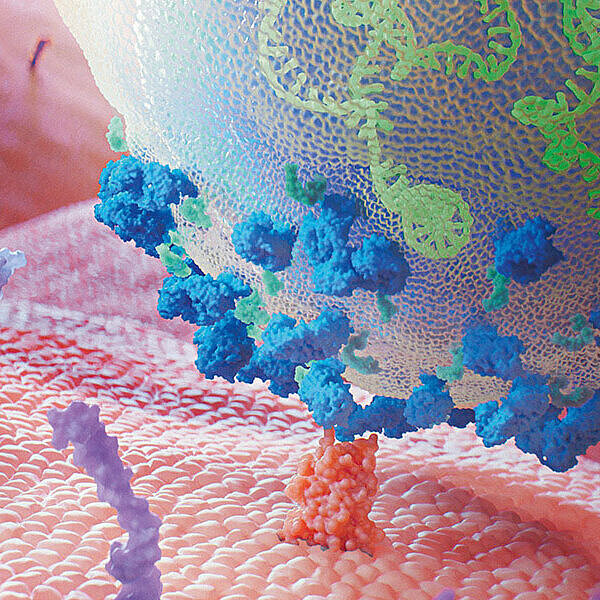
Sepsis is defined as a life-threatening organ dysfunction caused by a dysregulated host response to infection (1). Unlike the body’s immune response to ‘normal’, uncomplicated infection, sepsis not only fights the infection but also damages the body's own tissues and organs, leading to life-threatening organ failure. This systemic inflammatory response (SIR) leads to endothelial dysfunction with increased leukocyte adhesion and procoagulant changes which can progress to a thrombotic-inflammatory reaction called disseminated intravascular coagulopathy (DIC). DIC is an acquired syndrome characterised by the intravascular activation of coagulation with loss of localisation, causing damage to the microvasculature and occurs in approximately 35% of the cases. Sepsis is thereby the leading cause of infection-related deaths worldwide, with a mortality rate of 30−50% (2, 3, 4).
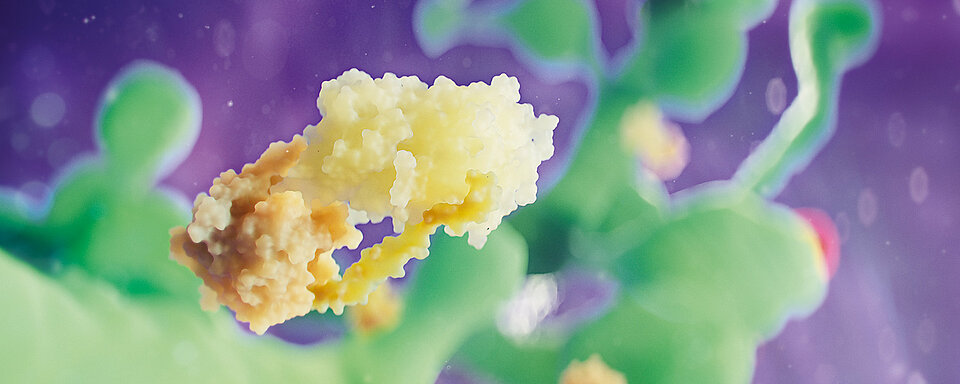
In sepsis-induced DIC, the release of inflammatory cytokines such as tumour necrosis factor (TNF) and interleukin-1 (IL-1) from the immune defence cells and the endothelium leads to the widespread production of tissue factor (TF) expression. The resulting activation of the extrinsic pathway is exacerbated by the downregulation of thrombomodulin (TM) expression on the endothelium, leading to diminished thrombin-mediated anticoagulation. At the same time, increased exposure of plasminogen activator inhibitor-1 (PAI-1), among others, leads to suppression of fibrinolysis. The increased coagulation activation with simultaneous inhibition of fibrinolysis causes microthrombi-related microcirculatory dysfunction and, in the further course, multi-organ failure. In this respect, it differs from DIC caused by other underlying diseases (e.g. tumours), as there is a greater tendency to bleed (3, 4, 5).
The rapid and reliable identification of sepsis and possible DIC are essential for the survival probability of the affected patients. In 2017, the Scientific and Standardisation Committee (SSC) of the International Society for Thrombosis and Haemostasis (ISTH) published an algorithm for identifying sepsis-induced coagulopathy (SIC) to complement the existing scoring system for DIC (3, 6). The proposed two-stage model will facilitate early recognition of DIC and potentially hasten the intervention (3). Patients with sepsis and platelet count of below 150 x 109/L should be examined using the SIC diagnostic criteria. These criteria include only three parameters, namely platelet count, prothrombin time (PT) and SOFA score (3, 4).
Patients who meet the criteria for SIC by the SIC score may be at risk of developing an overt DIC. Subsequently, the assessment of the overt DIC score is the proposed next step.
Like the SIC score, ISTH DIC score incorporates platelet count and PT but with different cut-offs. Fibrin-degradation products (FDP) / D-dimer and fibrinogen, but not the SOFA score, have been included in the ISTH DIC score to predict the presence of an overt DIC (3, 7). However, patients with sepsis typically have grossly elevated levels of fibrinogen. Consequently, these patients may have severe DIC despite normal, or even raised, fibrinogen levels.
In addition to the parameters recognised in the SIC and DIC score, other biomarkers have significant potential for the diagnosis and prognosis of sepsis and sepsis-related DIC. Antithrombin (AT) is considered as a sensitive marker for sepsis-induced DIC and can be used as a predictor for patient mortality. A strong reduction in AT together with decreased protein C and protein S levels without significant compensation during therapy, is an indicator of poor disease progression. Moreover, a reduced ADAMTS-13 activity, elevated PAI-1 and von Willebrand factor are often found in DIC, exhibiting certain prognostic power (4, 8, 9, 10).
Changes in the concentration of the plasma biomarkers − thrombin-antithrombin complex (TAT), soluble thrombomodulin (sTM), tissue plasminogen activator inhibitor complex (tPAIC) and plasminogen inhibitor complex (PIC) − may serve as an early indicator of DIC (8, 11, 12). However, the PIC level in patients with sepsis-related DIC is found differently in publications, hence supporting TAT, sTM and tPAIC as a reliable diagnosis of sepsis or sepsis-induced DIC that can be used together with the ISTH DIC score to assess patient's 28-day mortality (5, 13, 14). The determination of the TAT can exclude other diseases that could mimic DIC. TAT is elevated in patients with sepsis as a consequence of the coagulation process with predictive value. During the course of the disease, patients with moderate elevated levels and a faster normalisation of TAT concentration have a better prognosis than those with strongly increased TAT values. Additionally, patients with overt DIC have significantly higher levels than those who do not have an overt DIC.
On the other hand, both sTM and tPAIC are markers of endothelial dysfunction which is considered central to the progression to organ failure during sepsis (15). sTM levels are often elevated in patients with sepsis due to cleavage of endothelial thrombomodulin by leukocyte enzymes during SIR. In patients with poor prognosis, sTM levels are significantly higher compared to those with positive prognosis. Furthermore, tPAIC is associated with organ dysfunction caused by microthrombi and is therefore elevated in patients with sepsis. Patients with a poor prognosis often have elevated blood concentrations for much longer than patients with a positive prognosis (8, 11, 12, 13, 16).
References
(1) Singer M et al. (2016): The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 315(8): 801-810.
(2) Engel C et al. (2007): Epidemiology of sepsis in Germany: results from a national prospective multicenter study. Intensive Care Med 33(4): 606-618.
(3) Iba T et al. (2019): Diagnosis and management of sepsis-induced coagulopathy and disseminated intravascular coagulation. J Thromb Haemost 17(11): 1989-1994.
(4) Iba T et al. (2019): Diagnosis of sepsis-induced disseminated intravascular coagulation and coagulopathy. Acute Med Surg 6(3): 223-232.
(5) Asakura H. (2014): Classifying types of disseminated intravascular coagulation: clinical and animal models. J Intensive Care 2(1): 20.
(6) Iba T et al. (2017): New criteria for sepsis-induced coagulopathy (SIC) following the revised sepsis definition: a retrospective analysis of a nationwide survey. BMJ Open 7(9): e017046.
(7) Toh CH et al. (2007): The scoring system of the Scientific and Standardisation Committee on Disseminated Intravascular Coagulation of the International Society on Thrombosis and Haemostasis: a 5-year overview. J Thromb Haemost 5(3): 604-606.
(8) Hideo W et al. (1999): Hemostatic Molecular Markers Before the Onset of Disseminated Intravascular Coagulation. Am J Hematol 60(4): 273-278.
(9) Levi M et al. (2009): Guidelines for the diagnosis and management of disseminated intravascular coagulation. British Committee for Standards in Haematology. Br J Haematol 145(1): 24-33.
(10) Wada H et al. (2012): Guidance for diagnosis and treatment of disseminated intravascular coagulation from harmonization of the recommendations from three guidelines. J Thromb Haemost 11(4): 761-767.
(11) Kinasewitz GT et al. (2004): Universal changes in biomarkers of coagulation and inflammation occur in patients with severe sepsis, regardless of causative micro-organism [ISRCTN74215569]. Critical Care 8(2): R82-R90.
(12) Zhang J et al. (2021): Identification of soluble thrombomodulin and tissue plasminogen activator-inhibitor complex as biomarkers for prognosis and early evaluation of septic shock and sepsis-induced disseminated intravascular coagulation. Ann Palliat Med.
(13) Mei H et al. (2019): Evaluation the combined diagnostic value of TAT, PIC, tPAIC, and sTM in disseminated intravascular coagulation: A multi-center prospective observational study. Thromb Res 173: 20-26.
(14) Bouck EG et al. (2021): COVID-19 and Sepsis Are Associated With Different Abnormalities in Plasma Procoagulant and Fibrinolytic Activity. Arterioscler Thromb Vasc Biol 41: 401–414.
(15) Ince C et al. (2016): The Endothelium in Sepsis. Shock 45(3): 259–270.
(16) Innocenti F et al. (2019): Prognostic value of sepsis-induced coagulation abnormalities: an early assessment in the emergency department. Intern Emerg Med 14(3): 459-466.