Scientific Calendar December 2022
Which laboratory tests must be performed to diagnose LAD-III?
Assessment of the patient history, complete blood count, platelet aggregation tests by light transmission aggregometry (LTA), glycoprotein assessment of platelets using flow cytometry, and genetic analysis.
Platelet aggregation tests by light transmission aggregometry (LTA), glycoprotein assessment of platelets using flow cytometry, and genetic analysis.
Complete blood count, platelet aggregation tests by light transmission aggregometry (LTA) and glycoprotein assessment of platelets using flow cytometry.
Congratulations!
That's the correct answer!
Sorry! That´s not completely correct!
Please try again
Sorry! That's not the correct answer!
Please try again
Notice
Please select at least one answer
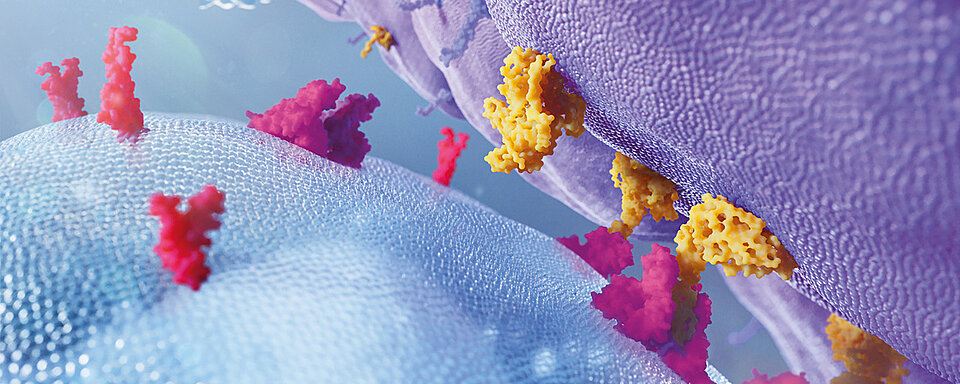
The leucocyte adhesion cascade
Under physiological conditions, the leucocyte adhesion cascade is initiated with leucocyte trapping and rolling on the endothelium, followed by chemokine-induced leucocyte activation, slow rolling, firm leucocyte adhesion and arrest, adhesion enhancement by integrin ligation, crawling and leucocyte transmigration.
Key molecular actors involved in adhesive processes include selectins and their glycoprotein ligands, chemokines and their receptors, integrins, and adhesion receptors of the immunoglobulin family. α4- and β2-integrin play a crucial role in the course of the cascade. Integrin activation occurs upon chemokine-triggered signalling (inside-out signalling) in cooperation with selectin-activated pathways. Activated integrins contribute to slow rolling, firm adhesion, crawling, and to transendothelial migration. [10]
The mutation of the ITGB2 gene (characteristic for LAD-I) causes a dysfunction of β2-integrin, which is no longer able to fulfil its function in the leucocyte adhesion cascade.
Clinical manifestation of the different LAD subtypes
The first symptoms of LAD appear during infancy or early childhood. [5]
Patients with LAD-I often experience life-threatening recurrent (bacterial or fungal) infections of the respiratory tract, skin and mucous membranes. The absence of typical signs of inflammation such as swelling, redness or pus formation at the site of infection is an important feature of LAD-I. Other indications of the presence of LAD-I include delayed detachment of the umbilical cord (after the 14th day of life), which often occurs only in association with infection of the umbilical cord stump, and delayed wound healing. [5, 11]
Mutations in the SLC35C1 gene (11p11.2), which codes for the guanosine-5'-diphosphate (GDP) fucose transporter localised in the Golgi apparatus, result in the clinical picture of LAD-II. This specific fucose transporter translocates GDP-fucose from the cytosol into the Golgi apparatus, where it is used as a substrate for fucosylation. The defective sugar transporter leads to impaired glycosylation of selectin ligands, which in turn leads to impaired recruitment and rolling of leucocytes. Patients with LAD-II often also have recurrent bacterial infections, but these are often less severe than those seen with LAD-I. Early tooth loss due to severe periodontitis as well as intellectual deficits and growth retardation characterise the clinical picture. LAD-II patients lack the H and Lewis Lea and Leb blood group antigens. [5, 9, 11]
The mutation in the FERMT3 gene (11q13.1) in patients with LAD-III results in a defect in the activation of all β-integrins (β1, β2 and β3), but normal integrin expression. This causes a clinical picture identical to that of patients with LAD-I. Additionally, due to the dysfunction of the β3-integrin, platelets are unable to adhere to the vessel wall, resulting in bleeding episodes similar to those of a patient with Glanzmann's thrombasthenia (GT). These patients tend to have longer bleeding episodes than healthy people and have more frequent nose and gum bleeds as well as bruises. [4, 5, 6, 7, 8, 11] Less than 40 cases of LAD-III have been reported so far. [12]
Diagnosis of LAD and its subtypes
The diagnosis of LAD includes the individual patient and family background as well as the examination of the blood count, platelet function and cell surface glycoproteins. A final diagnosis is always achieved by genetic analysis. [13]
The diagnosis of LAD-I is based on a quantitative complete blood count with evidence of neutrophilic leucocytosis. Decreased β2-integrin expression (CD11, CD18) in the leucocytes is detected by flow cytometry. Detection of ITGB2 mutations confirms the diagnosis. [13]
The diagnosis of LAD-II is based on clinical findings and a complete blood count with evidence of neutrophilic leucocytosis. Blood grouping is essential to detect for the Bombay blood group, which is present in all patients with LAD-II but not that often in the general population. The final diagnosis is based on genetic detection of mutations in the SLC35C1 gene (11p11.2). [9, 13]
The diagnosis of LAD-III is based on clinical findings and a complete blood count with evidence of neutrophilic leucocytosis. Platelet aggregation tests by light transmission aggregometry (LTA) using the agonists listed in Table 1 and surface glycoprotein analysis by flow cytometry (see Table 2) are employed for further diagnosis. [13] Distinguishing quantitative GT (type I and II) from LAD-III requires quantification of platelet glycoprotein expression by flow cytometry.
Table 1 Platelet aggregation in LAD-III per agonist [14]
| Agonist | Result |
| Epinephrine | Decreased / absent aggregation |
| ADP | Decreased / absent aggregation |
| Collagen | Decreased / absent aggregation |
| α-thrombin | Decreased / absent aggregation |
| TRAP6 | Decreased / absent aggregation |
| U46619 | Decreased / absent aggregation |
| CRP | Decreased / absent aggregation |
| Convulxin | Decreased / absent aggregation |
| PAR-4 ap | Decreased / absent aggregation |
| PAF | Decreased / absent aggregation |
| A23187 | Decreased / absent aggregation |
| Ristocetin | Normal response |
Table 2 Glycoprotein detection in LAD-III patients by flow cytometry
| Glycoprotein | Result |
| GPIIb (CD41) expression | Normal |
| GPIIIa (CD61) expression | Normal |
| GPIIb/IIIa activation epitope (PAC-1) | Defective activation |
In patients with LAD-III, the final diagnosis is achieved by genetic detection of the mutation in the FERMT3 gene (11q13.1). [13, 14, 15]
Therapeutic options
The treatment of patients is primarily limited to the control of infections with antibiotics and antimycotics. Patients with LAD-III may also receive transfusions, if needed. Currently, patients with LAD-I and LAD-III can only be cured by haematopoietic stem cell transplantation (bone marrow transplantation). Gene therapy may be a new therapeutic option for patients with LAD-I – studies are currently under way. [16, 17, 18] In patients with LAD-II, immune response can be improved by substituting fucose. [19] These patients generally have a significantly longer life expectancy than patients with LAD-I and LAD-III.
Leucocyte adhesion deficiency (LAD)
Leucocyte adhesion deficiency (LAD) syndromes are a group of rare primary immunodeficiencies classified into three subtypes: LAD-I, LAD-II and LAD-III. All three are characterised by marked leucocytosis, impaired leucocyte adhesion and recurrent infections. [1, 2, 3, 4]
LAD is caused by a gene defect which is inherited in an autosomal recessive manner. LAD-I is caused by mutations in the ITGB2 gene (21q22.3), which codes for the β2-integrin CD18. [2, 5] LAD-II is caused by a mutation in the SLC35C1 gene (11p11.2), which codes for the guanosine 5'-diphosphate (GDP) fucose transporter, and LAD-III results from a mutation in the FERMT3 gene (11q13.1), which codes for kindlin-3 of haematopoietic cells. [5, 6, 7, 8, 9] These mutations result in impaired cell adhesion, which leads, among other things, to restricted cell migration from the vessels to the site of infection. [6, 7, 8, 9]
References
[1] Etzioni A et al. (1992): Recurrent Severe Infections Caused by a Novel Leukocyte Adhesion Deficiency. N Engl J Med; 327: 1789–1792.
[2] Anderson DC, Springer TA. (1987): LEUKOCYTE ADHESION DEFICIENCY: An Inherited Defect in the Mac-I, LFA-l, and pI50,95 Glycoproteins. Ann Rev Med; 38: 175–194.
[3] Mathew EC, Shaw JM, Bonilla FA, Law SK, Wright DA. (2000): A novel point mutation in CD18 causing the expression of dysfunctional CD11/CD18 leucocyte integrins in a patient with leucocyte adhesion deficiency (LAD). Clin Exp Immunol; 121: 133–138.
[4] Kuijpers TW et al. (1997): Leukocyte adhesion deficiency type 1 (LAD-1)/variant: a novel immunodeficiency syndrome characterized by dysfunctional β2 integrins. J Clin Invest; 100: 1725–1733.
[5] Hanna S, Etzioni A. (2012): Leukocyte adhesion deficiencies. Annals of the New York Academy of Sciences; 1250: 50–55.
[6] McDowall A et al. (2003): A novel form of integrin dysfunction involving β1, β2, and β3 integrins. J Clin Invest; 111: 51–60.
[7] Svensson L et al. (2009): Leukocyte adhesion deficiency-III is caused by mutations in KINDLIN3 affecting integrin activation. Nat Med; 15(3): 306–312.
[8] Meller J et al. (2012): Novel aspects of Kindlin-3 function in humans based on a new case of leukocyte adhesion deficiency III. J Thromb Haemost; 10: 1397–1408.
[9] Hidalgo A et al. (2003): Insights into leukocyte adhesion deficiency type 2 from a novel mutation in the GDP-fucose transporter gene. Blood; 101(5): 1705–1712.
[10] Mitroulis I et al. (2015): Leukocyte integrins: Role in leukocyte recruitment and as therapeutic targets in inflammatory disease. Pharmacol Ther; 147: 123–135.
[11] Harris ES, Weyrich AS, Zimmerman GA. (2013): Lessons from rare maladies: leukocyte adhesion deficiency syndromes. Curr Opin Hematol; 20(1): 16–25.
[12] Saultier P, Szepetowski S, Canault M et al. (2018): Long-term management of leukocyte adhesion deficiency type III without hematopoietic stem cell transplantation. Haematologica; 103(6): e264–e267.
[13] Etzioni A. (2007): Leukocyte Adhesion Deficiencies: Molecular Basis, Clinical Findings, and Therapeutic Options. In: Shurin MR, Smolkin YS. (eds.) Immune-Mediated Diseases. Advances in Experimental Medicine and Biology. Vol. 601; Springer, New York, NY.
[14] Gresele P for the Subcommittee on Platelet Physiology. (2015): Diagnosis of inherited platelet function disorders: guidance from the SSC of the ISTH. J Thromb Haemost; 13: 314–322.
[15] Manukjan G et al. (2020): Novel variants in FERMT3 and RASGRP2—Genetic linkage in Glanzmann-like bleeding disorders. Pediatr Blood Cancer; 67: e28078.
[16] Almarza E et al. (2019): Gene Therapy for Lad-I Immunodeficiency: Preclinical Evaluation of HSC Transduction Under Optimized GMP-Conditions. Blood; 134 (Supplement_1): 5751.
[17] Mesa-Núñez C et al. (2022): Preclinical safety and efficacy of lentiviral-mediated gene therapy for leukocyte adhesion deficiency type I. Molecular Therapy - Methods & Clinical Development; 26: 459–470.
[18] Kohn DB et al. (2021): A Phase 1/2 Study of Lentiviral-Mediated Ex-Vivo Gene Therapy for Pediatric Patients with Severe Leukocyte Adhesion Deficiency-I (LAD-I): Interim Results. Blood; 138 (Supplement_1): 2932.
[19] Marquardt T et al. (1999): Correction of Leukocyte Adhesion Deficiency Type II with Oral Fucose. Blood; 94(12): 3976–3985.